I am a senior orthoptist in the University Hospital of Wales (UHW) in Cardiff. Not many people have heard of orthoptists or have any idea what we do, but I’d like to think, for lots of people, we are invaluable.
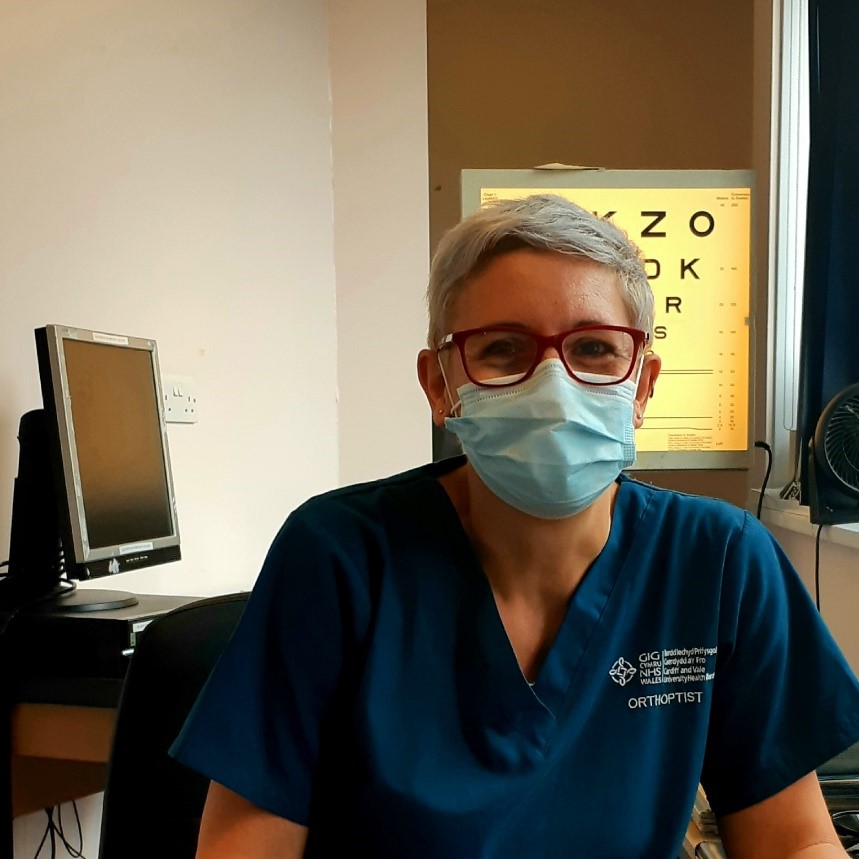
Emma Tippings
We work in hospitals that have an eye clinic. We investigate and treat patients of all ages. Our speciality involves something called binocular vision. In other words, using your eyes together.
Any child with an eye problem that results in them ‘preferring’ to use one eye in favour of the other eye, are at risk of developing a ‘lazy eye’. This means the vision does not develop as well in the problem eye because the eye is not used sufficiently. Some of the more common reasons for this are having a stronger need for glasses in one eye, having an eye that turns, having a problem with the back of the eye (the retina) or perhaps the lens in the eye (e.g. a cataract).
Some children are born with these conditions and others develop them later in childhood. All these children will need treatment to encourage them to use their lazy eye. We do this by covering their good eye with a patch or putting drops in their good eye to blur it in a hope they will use the other eye. The investigations and treatment for these children are carried out by orthoptists.
Quite a lot of the children we see have an eye that turns. The medical word for this is a strabismus. It is the job of the orthoptist to identify the strabismus and classify it so, as well as treatment to improve the vision such as patching, the appropriate treatment for aligning the eyes can be undertaken. This usually involves glasses, surgery or a combination of both.
At times the reason for poor vision or a strabismus can be very serious. In some cases, the vision of the child may not be retrievable, or the cause of their eye problem may be related to a life changing/limiting condition. As orthoptists we often have to prepare and counsel the parents/children/teenagers regarding their prognosis.
Our adult patients also have problems using their eyes together. Some of them would have been patients of the orthoptic clinic as a child and had previous treatment for a strabismus when younger. The position of an eye can change with time so they may seek referral to investigate whether further surgery can be undertaken to re-align their eyes into a better cosmetic position.
A bigger portion of our adult workload probably consists of patients who have a sudden onset strabismus. If they previously had straight eyes, then this new condition will result in them experiencing double vision. This is because they will perceive an image of what they are looking at with their straight eye, but also an image of something else with their turning eye.
These patients are usually referred to us as an emergency either by their optometrist, GP or another department within the hospital. They need to be investigated because the cause of a sudden onset strabismus is often very serious. It is the role of the orthoptist to try and identify this cause. It can be related to other health conditions the patient may have but is often neurological in origin. Age and associated symptoms can help us identify it.
Our findings and thoughts on potential diagnosis leads to decisions on what further investigations need to be performed such as blood tests and CT/MRI scans, and also how urgent these need to be done. We are often the first health professional this group pf patients see in the hospital. Therefore, empathy and the ability to explain things carefully to these patients is needed. They are often extremely worried about what the future has in store for them both visually, and generally.
As orthoptists we can also help with their symptoms of double vision. We can use prisms that we fit to the patients’ glasses to try and alleviate their double vision, or we can cover one eye with a patch or cover one lens of their glasses to prevent the double vision being noticed. If you are only using one eye, you will only see one image.
My role in UHW is the adult lead for orthoptic services so the majority of my workload is adult patients. Orthoptists are based in the out-patients clinic. I work closely with the ophthalmologists in the eye clinic especially those who specialise in neuro-ophthalmology and the doctors in eye casualty. We also advise the neurology department and those in the maxillo-facial department, on patients they ask us to assess. We are routinely involved in a multi-disciplinary approach to patient care.
I have been working at UHW for over 25 years and really enjoy my job. We see a wide variety of patients with lots of different problems and our main aim is to diagnose their condition and hopefully treat them successfully. Along their journey we try and make them as comfortable as possible and reassure them as best we can.